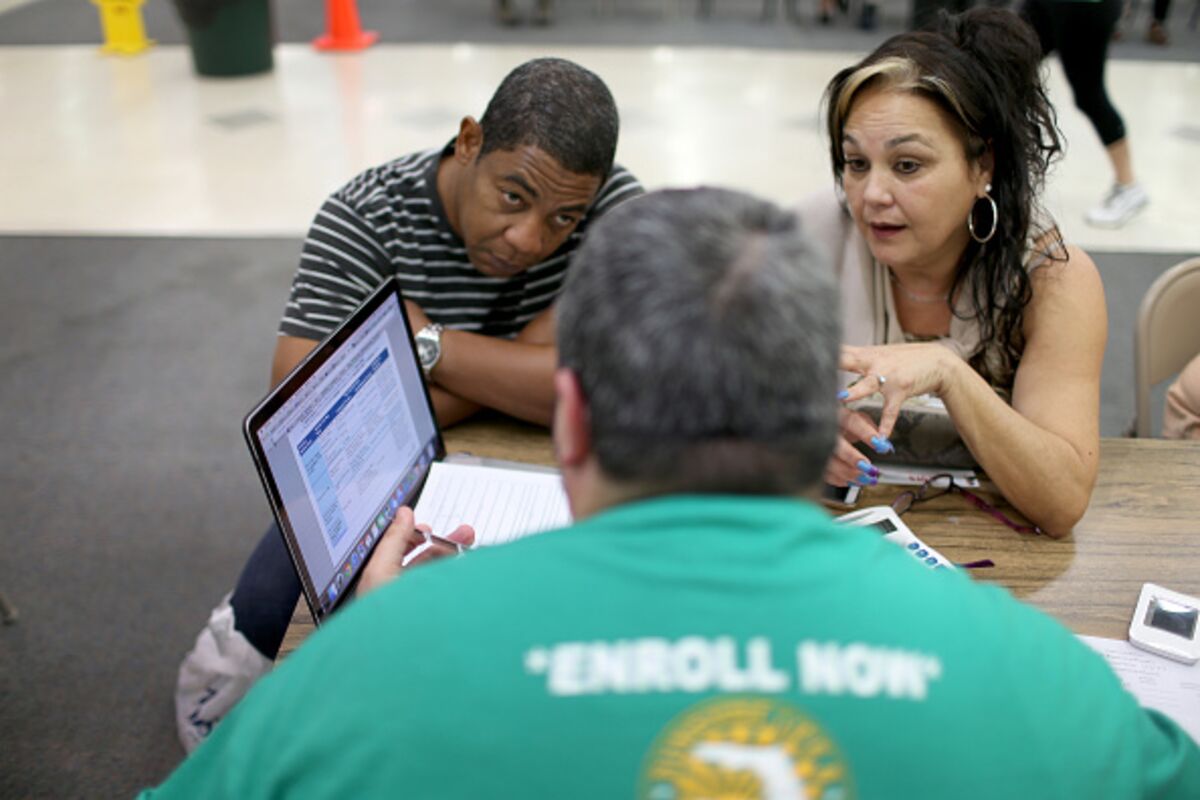
People discuss plans available from the Affordable Care Act at a store setup in the Mall of the Americas on Dec. 15, 2014 in Miami, Fla.
At the Coastal Carolina Fair outside Charleston, S., you can visit a haunted house, touch a llama at the petting zoo, and, until this year, sign up for health coverage under the Affordable Care Act. Workers from the nonprofit Palmetto Project sometimes stayed at the fairgrounds until midnight over the past four years to help people enroll, but they won’t be there Thursday when the fair opens. The Trump administration cut the group’s $1 million federal grant in half, part of a broader push by the White House to weaken promotion for the marketplaces.
The four-year-old Obamacare marketplaces will face their toughest year yet when the window to buy coverage opens on Nov. Already, even before enrollment opens, President Donald Trump has halted payments to insurers that reimburse them for reducing out-of-pocket costs for low-income people. That means those who turn up seeking health coverage, despite the steep cuts to outreach and marketing and an abbreviated enrollment period, will face even higher premiums. The combination is likely to depress the number of people who purchase health plans, although no one can predict by how much.
The number of people who signed up during open enrollment last year declined by about 4 percent, or 466,000 for 2017, compared to 2016 levels. About 60 percent of current marketplace customers didn’t know when enrollment begins, according to a Kaiser Family Foundation poll released Oct. Among the uninsured, 85 percent were in the dark.
The Obama administration tried to maximize sign-ups for its signature domestic achievement, routinely sending President Obama out to promote the law in late-night TV appearances and on viral videos. Now the momentum of the White House swings in the opposite direction. “Obamacare is finished,” Trump said at an Oct. 16 cabinet meeting, three weeks after the Republican-controlled Senate failed to repeal the law. “It`s dead. It`s gone. It`s no longer—you shouldn`t even mention it. It`s gone. There is no such thing as Obamacare anymore.”
The Affordable Care Act remains the law, of course, but that doesn’t mean the president can’t convince people otherwise. “The president has said Obamacare is dead,” says Christine Eibner, a senior economist at RAND Corp. “What do people think when they hear that?”
It makes insurers nervous. Independence Blue Cross insures about 300,000 people in the individual markets of Pennsylvania and via an affiliate in New Jersey. Chief Executive Dan Hilferty is increasing advertising and outreach, which could offset some of the federal cuts, but he still expects enrollment to drop because of higher prices and an overall sense of uncertainty emanating from Washington. “Sometimes, people aren`t even sure if coverage is going to be offered,” he says.
Health Care Service Corp., the parent of Blue Cross and Blue Shield plans in Illinois, Texas, and three other states, says it`s airing new ads this year to make sure customers know the enrollment period is shorter. Another insurer, Blue Cross and Blue Shield of Florida, is using direct mail and in-person outreach to remind customers that “the ACA is still here, the plans are still available,” says Jon Urbanek, the company`s senior vice president of health insurance markets.
Competition was dwindling and prices were rising, even before Trump won the election. Nearly half of enrollees will have just one or two insurance companies to pick from for next year’s coverage, according to data compiled by Bloomberg. Rates are going up about 30 percent on average, according to ACASignups.net, though the law’s subsidies insulate about half of enrollees from higher sticker prices.
The Department of Health and Human Services blames the Obama administration for higher premiums and insurers leaving the market. “The previous administration inflicted heavy damage on the individual market,” spokesman Matt Lloyd said in a statement. Trump signed an executive order to eventually encourage enrollment in cheaper short-term health plans and other policies that offer less coverage that ACA plans, a move “intended to provide Americans with more affordable health care choices,” Lloyd added.
But some of the administration’s actions look like they’re intended to make choosing ACA plans more difficult. Besides cutting funding to outreach groups like Palmetto Project, the Trump administration lopped a zero off the overall advertising budget, reducing it to just $10 million from $100 million last year. The enrollment period has been 12 weeks long in each of the past three years, but in most states it’s shrinking to six weeks.
If fewer people enroll, "the risk pool will probably get worse," says Benjamin Sommers, health economist at the Harvard T. Chan School of Public Health. The cuts to advertising alone will decrease 2018 enrollment by at least 1.1 million people, estimates Joshua Peck, who was chief marketing officer for healthcare.gov during the Obama administration and has since co-founded a group urging people to sign up for ACA plans.
One federal action may boost enrollment. The IRS, which administers the ACA’s tax penalties for people who forgo health insurance, said this month that it would not accept 2017 tax returns that don’t indicate whether the filer had insurance. That signals a stricter enforcement of the ACA’s individual mandate than many had expected under Trump.
Roughly half of the 17.5 million Americans who buy health insurance on their own don’t receive federal subsidies, according to Kaiser, and often feel the pain of rising premiums and out-of-pocket costs. Laura McCrea, a 58-year-old retired sales manager in Louisville, Ky., pays $519 a month for an ACA plan from Anthem Inc. and doesn’t qualify for subsidies. “We’re the ones who are going to get hit really hard,” she says. McCrea needed a heart catheterization test this year and had to pay $5,000 before her insurance kicked in. She says she supports the ACA but wants a fix to bring down costs.
While each state’s marketplace is different, there are signs that health plans had raised prices enough in recent years that the market had stabilized in 2017. Insurers’ profits on individual plans, before counting administrative costs, more than doubled in the second quarter of 2017 compared to the same period last year, according to a Kaiser Family Foundation analysis.
But if plans enroll fewer people this year, that stability may be short-lived. Miranda Brown, the outreach coordinator at the Kentucky Equal Justice Center, has already seen how confusion and a decline in government support can affect the health law. After Republican Governor Matt Bevin took over from his Democratic predecessor, he ended the state`s Kynect insurance marketplace last year, sending Kentuckyians to healthcare. Enrollment in Kentucky dropped by about 15 percent in 2017.
“From the beginning Kynect really did a lot of advertising and promotion around town,” Brown says. “Now there’s hardly any signs that this is something going on that impacts people.


0 comments:
Post a Comment